MED-EL
Published Jun 27, 2018
Individualized Cochlear Implants: Prof. Paul Van de Heyning
Today is truly a remarkable day in the field of hearing implants and beyond. We’re excited to announce the dawn of a new era in cochlear implants: Individualized CI.
We are honored to have Prof. Dr. Paul Van de Heyning here to give you an in-depth look at the incredible potential of individualized CI.
This will be a turning point—a turning point in the field of individualized medicine. The time of getting an electrode or an implant and just getting it in the patient, that that was enough. This time is over.
No patient is alike, no person is alike, and we have to respect that, and we have to step forward now—step forward in this individualized medicine. –Prof. Dr. Paul Van de Heyning
Prof. Van de Heyning is the Chairman of CI2018, the 15th International Conference on Cochlear Implantation and Other Implantable Technologies, and he is a Professor and Chairman at the Department at Otorhinolaryngology and Head and Neck Surgery from the Antwerp University Hospital.
Today, Prof. Van de Heyning is sharing his clinical experience with OTOPLAN, the surgical planning platform that is the key to individualization.
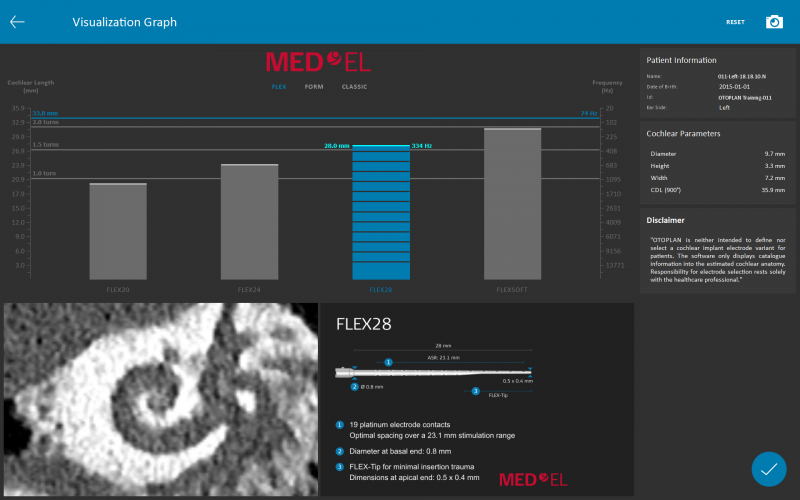
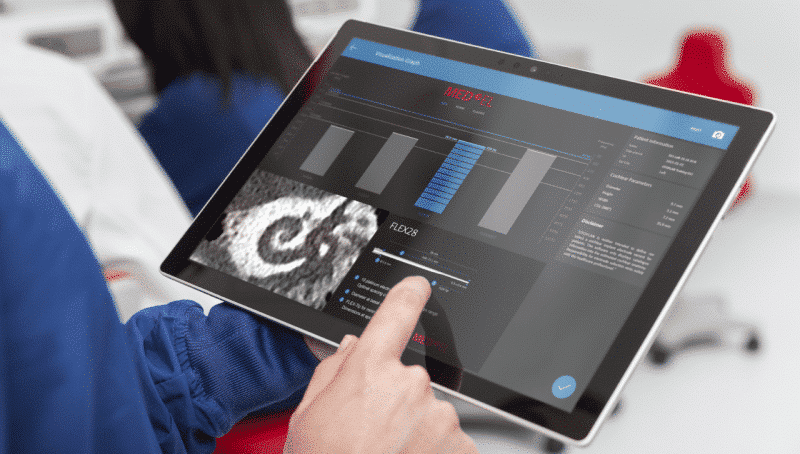
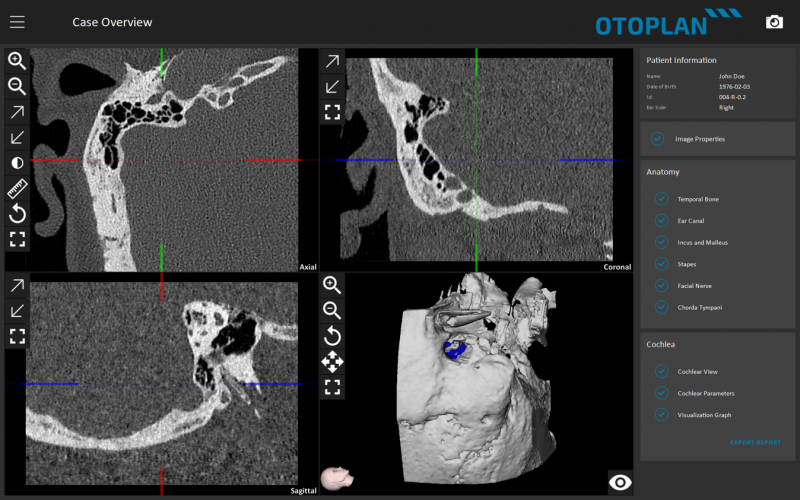
OTOPLAN is a revolutionary tablet-based planning software that lets you quickly create patient-specific 3D reconstructions from medical imaging. This intuitive platform provides incredible 3D visualization in a portable platform. With OTOPLAN, you can easily visualize each patient’s unique anatomy and choose the optimal electrode array for each individual patient.
Let’s go over to Prof. Van de Heyning to hear his experiences with OTOPLAN and individualized cochlear implants.
OTOPLAN: The Key to Individualized CI
OTOPLAN gives us now more freedom to plan our surgery. The program allows us to load the detailed data from the radiologists and then to have a look at these images from our own perspective. It allows us to do more precise measurements, it allows us to get a better idea on the anatomical difficulties that we might encounter during the surgery.
And for the implantology, it allows us to better choose which electrodes, which implant to use for this particular patient. It allows us also to have a better planning in these patients.
So to summarize, it is a more individual approach for us. It’s a tool that helps us in doing this in the future and to give this particular surgical look at radiology. And this is different from the perspective of the radiologists. The radiologist looks at the diagnostic viewpoint on the pictures, but now we can look at it from the surgical view.
Can’t See This Video?
Having problems viewing this video? Watch it on YouTube.
Instant 3D Visualization
I would definitely advocate OTOPLAN to a surgeon, because this allows you to get this individualized medicine to do so more with your radiology. We need high quality of pictures, we need good diagnosis. For that we need good radiologists. Good radiologists with whom you’re working with give you a better outcome. And OTOPLAN is a step further.
To be honest, we are always a little bit frustrated by the pictures we get from the radiology, because we want to look in these pictures, or to do with these pictures so much more than the mere diagnosis, or the pictures we get, or the incidents we get from the radiologist. And we were in fact unable to do that.
Okay, we could ask to our fellow radiologists once, “Oh, could you do this series or that incidents, I’m coming to you office?” and with the mainframe PCs of radiologists, you can do 3D reconstructions, but that is doing something exceptionally, that is costing a lot of time. I know you can do it once, but not two times and certainly not ten times.
When the radiologist has done their work, then OTOPLAN starts. Then our work starts. How are we now translating this information in our strategy to treat the patient. Not only the diagnosis, but on choices of electrodes, on choices of surgical approaches, on to look of it how we might encounter particular difficulties during the surgery and how we can plan our trajectory through the temporal bone for our surgery.
And last but not least, we have this 3D. You could say there’s a very high risk in this program, because it is highly addictive. It’s just fun to do that and to plan this, using this. It’s not a nuisance. There were programs that were difficult to handle, but is inviting you to do it.
And OTOPLAN, I just know I like it. I just know I like it. It allows you, just in a few minutes to get the 3D view, this really individualized anatomical data, you can measure on it, in different directions, so it adds so much to your radiology. That soon when you’re acquainted with the program, you cannot miss it.
Individualization: Better Surgical Outcomes
Surgery is always an individualized thing. No one has the same anatomy, no one has the same risks, and each time that you do surgery, you have to explore a little bit, the variations that nature has given in each of us. And there’s quite a lot of variation. When we look at text books and it looks as if everything is the same, but this is not real life.
Real life is that we encounter huge variations where the facial nerve is or where the ossicles are, and on pathology. Having the possibility that you can anticipate that, that you can foresee this, that you don’t have to find it out during your surgery, with a tool that is easy to use and allows you to prepare your surgery is of a great help.
Individualization is a hot topic, but here it has a real meaning. Instead of speaking and discussing in general terms, or preparing a surgery in general terms, we can make it much more individualized.
We did an introduction of OTOPLAN in a group of HEARRING, of the HEARRING members, and we presented the possibilities of this OTOPLAN system, and we asked, “What do you think that it will help you in first place?” And before choosing electrode whatever, everyone said, point number one was we’ll have a safer surgery.
When you’re dealing with congenital anomalies, then every experience is different, because none of the children have the same cochlear. Each of them have some anatomical malformations of order, dispositions that we did not anticipate normally, and then to find out during the surgery, now we can do it ahead. We can plan our surgery and look what are the different structures we have to avoid. And can for sure make much progression in the surgery.
And of course this will reduce in a large amount also the risk of complications. This is more pronounced when you have to do with very exceptional anatomical situations or that it is re-do surgery, or there are congenital anomalies, or it is after trauma. There are wide variations of situations that are hard to predict and this allows you to predict particular aspects of your surgery.
Patient-Specific Surgical Planning
I think about a particular child with a congenital malformation, which is very hard to do, due to these very extreme anomalies in that particular child. And it helped us a lot to have the proper approach, because there was no normal anatomical landmark to be able to recognize. We had to map the facial nerve by electro-stimulation. The facial nerve was lying on a place where we normally would enter the cochlear, so we had to find this entrance. And the way that we were able to look at it during the surgery by manipulating the program, was a great help to complete the surgery in a good way, in a successful way, and being able to introduce the electrodes in the cochlear in a proper way.
And to be honest, in a broader perspective, in fact it helps us in every surgery. We want to have better hearing preservation and we discuss a lot on an ideal way the electrode should be introduced in the scala tympani. Just thinking of how the insertion angle would be, into something that you cannot see because you see the round window, but the precise angle of the scala you cannot see.
Now you can program it before and have a good idea. You do, in fact, virtual computer-assisted surgery and it helps us in defining what is the optimal trajectory, and then you can mimic that. And bring your electrodes in, in the right direction. This is only by, before the surgery, to have a virtual image of that, to mimic that virtual image during the surgery. And OTOPLAN allows you to do that.
Individualized Electrode Choice
Well, up to now when we were doing cochlear implantation and in particular this type of surgery, we used a standard electrode, one electrode for all the patients. So it’s like going to a shoe shop and saying one size fits all. This time is over.
We know that when we adapt our choices of electrodes and implants to the individual situation of a patient that we can reach much better results. So this OTOPLAN is a tool that allows us to implement real personalized medicine, individualized medicine, and can then very much better provide what the patient needs and what we particularly want for them.
When we discuss with a patient the surgery, we have to discuss the different options. The options are, are we choosing to do a deep insertion of the electrodes, do we want that the tip electrodes are far inside the cochlear, can stimulate the second turn of the cochlear, to get what’s called the full cochlear coverage, or on the contrary, with patients with residual hearing where we want to keep the residual hearing and where we do not want that electrodes are getting into this residual hearing zone, these are fundamental options and choices.
Then it’s time to implement. And we have to make the right choice, because not everyone has the same cochlea. It’s not that one electrode, because before it was one electrode for every cochlea, but we know there’s a huge variation in sizes from cochlear lengths. The organ of Corti, the cochlear duct length varies from 25– 36 millimeters, really this is a 50% change, from one patient to another patient.
So we have to calculate if we want to reach the second turn, what is the length necessary to get there. A short electrode might be enough in someone with a small cochlea, and a long electrodes is of course necessary for patients with a large cochlea. But if we would use a large electrode and want just to stimulate in the basal turn and not to stimulate in the apical turn, then a long electrode would be the wrong choice.
Individualized Hearing Preservation
A hot topic in cochlear implantation is to preserve inner ear function. It is important to preserve this in those patients that have residual hearing, because it contributes to speech comprehension, to music and speech quality, and to do that, to allow that, we have to precisely match electrode length and insertion depth into the cochlear. We do not want to have an electrode depth that extends too far in the cochlear in this particular situation, because then we jeopardize the inner ear structure of the second turn and the cochlear.
Instead of, in the past, speaking of how many millimeters we want to insert an electrode, now it’s time to shift to how many degrees with to insert it. This needs this individual match between the real cochlea of this particular patient, not the average one, this particular patient, and the actual choice of our electrodes.
And so we need for a particular patient to define what is the insertion length to insert it. We can calculate if we define, oh we want to stimulate not beyond 500 Hz. 500 Hz corresponds to something like 400 degrees. We want to insert 400 degrees, how many millimeters do we know, and this program helps us in doing this calculation and this estimation of insertion depth of the electrode.
OTOPLAN will help us in many ways. It will help us in many ways because we can individualize the choice of the electrode length in cochlear implantation. If we limit the advantage for patients now to cochlear implantation, then OTOPLAN will allow us to do a better choice of electrode in a particular patient. We will be able to set up our goals and to act accordingly.
And if we want to have a deep insertion, to calculate which length of electrode do we need, and if this patient with residual hearing and wants to keep that, then we need shorter electrodes, and we can also calculate, or it helps us calculating which is the particular electrode which is needed.
Anatomy-Based Fitting
This is a huge advantage that we can individualize the choice of this electrode lengths. This is the first part. And then, there’s another element that is provided by the OTOPLAN program and this element helps the audiologists.
We can anticipate when we use a particular electrode in a particular cochlear, what will be the right frequency allocation for each electrode, and what is the optimal frequency band to be programmed to that particular electrode contact. In the Greenwood function, we know at which angle of insertion in the cochlea a particular frequency is located and matching that to the electrode that will be implanted is a great advantage. And moreover, we can fine-tune it after surgery by doing a new CT scan. And then define the actual insertion angle of a particular electrode to this fitting program.
And when the surgery is done and we achieve these goals, then we will have better frequency allocation. So the way of fitting the implant to the actual location of the electrodes in the cochlear and all these facts together, will give clearer step forward again in speech recognition in patients, and also in appreciation of music and auditory capability at large.
Individualization: The Future of Cochlear Implants
This will be a turning point—a turning point in the field of individualized medicine. The time of getting an electrode or an implant and just getting it in the patient, that that was enough. This time is over.
This will be remembered as the point of individualized medicine, where a particular patient has his or her context, his or her anatomy, his or her audiometric capabilities, communication, interactions, and taking all that in turn, taking the proper choice. The proper choice of implant. The proper choice of electrodes. The proper choice of surgical techniques. The proper choice of rehabilitation.
No patient is alike, no person is alike, and we have to respect that, and we have to step forward now—step forward in this individualized medicine.
Thank you for sharing your experiences Prof. Van de Heyning, we look forward to hearing more from you and your team soon.
Subscribe & Share
Ready to learn more about individualized cochlear implants?
Check out this article to see how OTOPLAN works. Or find out what sets MED-EL flexible lateral wall arrays apart from any other electrode arrays.
Want to see Prof. Van de Heyning’s structure preservation surgical techniques in crystal clear HD? Check out this great video case study!
*Not all products, indications, and features shown are available in all areas. Please contact your local MED-EL representative for more information.
MED-EL
Was this article helpful?
Thanks for your feedback.
Sign up for newsletter below for more.
Thanks for your feedback.
Please leave your message below.
CTA Form Success Message
Send us a message
Field is required
John Doe
Field is required
name@mail.com
Field is required
What do you think?
The content on this website is for general informational purposes only and should not be taken as medical advice. Please contact your doctor or hearing specialist to learn what type of hearing solution is suitable for your specific needs. Not all products, features, or indications shown are approved in all countries.
MED-EL