MED-EL
Published Apr 12, 2017
Reducing the Risk of Cochlear Implant Electrode Array Deviation
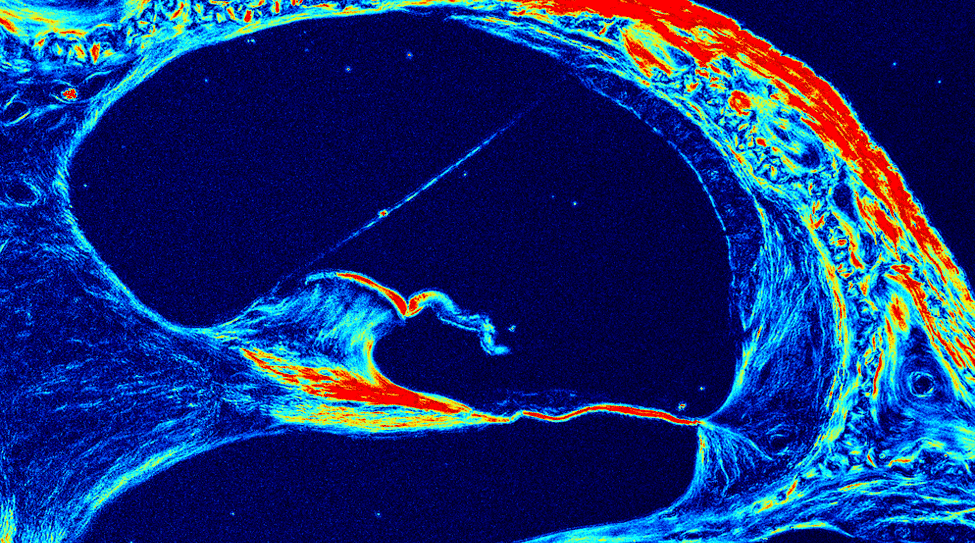
Image courtesy of SPIE Publications & Kalwani et al. (2013).
In part one of this series on electrode array deviation, we looked at how cochlear structures can be damaged when an electrode deviates from the scala tympani into the scala vestibuli.1 This can have a substantial effect on patient outcome, including complete loss of residual hearing, pitch confusion, and significantly lower speech perception scores.1,2,3,4,5
Scala tympani placement isn’t always possible for every patient, but more consistent placement has clear benefits.1 So how can you reduce the risk of having an array deviate from the scala tympani to the scala vestibuli?
In this post, we’ll look at two factors that are associated with a significantly increased risk of damage to cochlear structures, and how you can avoid both of these risk factors.
Round Window vs. Cochleostomy
First, let’s look at how surgical approach can have a significant effect. A cochleostomy can lead to a higher likelihood of electrodes in the scala vestibuli. Round window technique has demonstrated much better prospects of having electrodes fully in the scala tympani.4,5,6
Wanna et al. (2014) found that a cochleostomy approach lead to electrodes in the scala vestibuli significantly more often, even when controlling for array design.4
- Cochleostomy (n=38): 36.8% fully in scala tympani
- Extended Round window (n=43): 83.7% fully in scala tympani
- Round Window (n=35): 91.5% fully in scala tympani
Even for experienced surgeons, there can be a high degree of variability with a cochleostomy.7 This may be a reason for more consistent scala tympani placement with round window and extended round window insertions.1,4,5 In addition to more consistent placement, round window insertion has also been significantly associated with the absence of hydrops and fibrosis of the inner ear, in comparison to cochleostomy.8
Lateral Wall Arrays vs. Perimodiolar Arrays
However, surgical approach isn’t the only significant factor in electrode array deviation. Several recent studies have found that electrode array deviation is far more likely with perimodiolar or mid-scala electrode arrays.1,4,5,9
O’Connell et al. (2016) found that compared to lateral wall arrays, perimodiolar arrays and mid-scala arrays were far more likely to enter the scala vestibuli.5
- Perimodiolar arrays(n=106): 48.7% fully in scala tympani
- Mid-scala arrays(n=14): 42.9% fully in scala tympani
- Lateral wall arrays (n=93): 95.7% fully in scala tympani
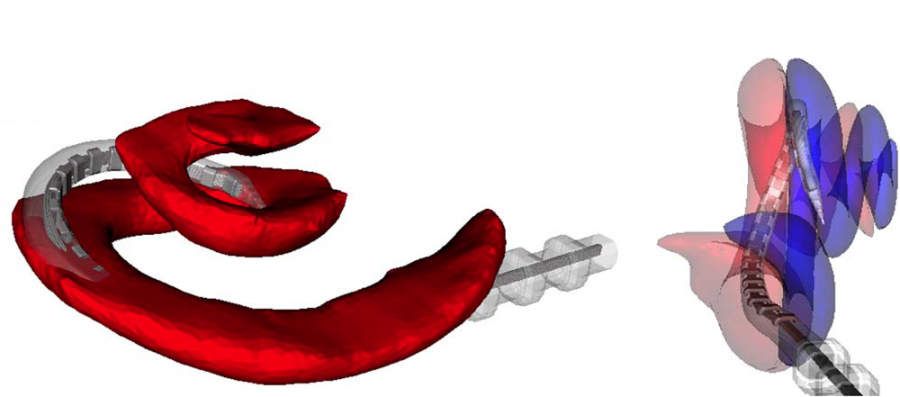
Fig. 1: Reconstructed CT images from Wanna et al. (2014) showing translocation of a perimodiolar electrode array from the scala tympani into the scala vestibuli. The perimodiolar electrode array crosses the basilar membrane and exits the scala tympani (red) in the basal turn, and deviates to the scala vestibuli (blue). Image used with permission from Wiley Publishers.
Optimal Electrode Array Placement
Taking both array design and surgical approach into consideration, it’s reasonable to conclude that the ideal array for scala tympani placement would be:
- A flexible lateral wall array
- Optimized for round window insertion
It’s possible to achieve consistent scala tympani insertions with the combination of flexible lateral wall arrays and round window insertion.
Nordfalk et al. (2014) utilized flexible MED-EL lateral wall arrays and a round window approach. Post-op CT of 29 patients showed all 29 arrays were located fully within the scala tympani.7
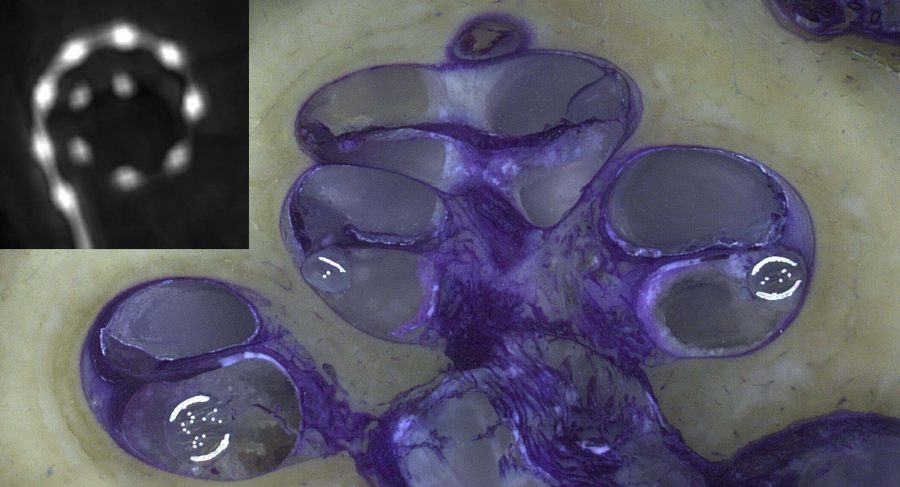
Fig. 2: Flexible MED-EL lateral wall electrode array placed fully within scala tympani using round window approach. Image courtesy of Peter Erfurt & Prof. Dr. Thomas Lenarz, MHH Hannover, Germany.
Avoiding electrode array deviation isn’t always possible—but significantly better rates of successful scala tympani placement can be achieved with the combination of soft surgical techniques and flexible lateral wall arrays.
For your patients, this supports much better hearing performance:
- Accurate electrode mapping 1,2
- Significantly better speech understanding 4,5
- Intact cochlear potential for future therapies
By choosing flexible MED-EL arrays and round window insertion, you can better avoid the risks associated with cochleostomy and perimodiolar arrays.
Looking for more insight on round window insertion techniques and flexible MED-EL arrays? Check out our MED-EL Surgical Video Library for high-definition surgical case studies with expert surgeons demonstrating their techniques.
Get the latest MED-EL Professionals Blog posts straight to your inbox—subscribe right now.
*Not all products, features, and indications shown are available in all areas. Please contact your local MED-EL representative for more information.
References:
Cover: Image used with permission from SPIE Publications and authors. Kalwani, N.M., Ong, C., Lysaght, A.C., Haward, S.J., McKinley, G.H., & Stankovic, K.M. (2013) Quantitative polarized light microscopy of unstained mammalian cochlear sections. J. Biomed. Opt. 0001;18(2):026021-026021. doi:10.1117/1.JBO.18.2.026021.
Fig. 1: Image used with permission from Wiley Publishers and authors. Wanna, G. B., Noble, J. H., Carlson, M. L., Gifford, R. H., Dietrich, M. S., Haynes, D. S., Dawant, B. M. & Labadie, R. F. (2014). Impact of electrode design and surgical approach on scalar location and cochlear implant outcomes. The Laryngoscope, 124: S1–S7. doi: 10.1002/lary.24728
Further usage of any Wiley content that appears on this website is strictly prohibited without permission from John Wiley & Sons, Inc. Please contact Wiley’s Permissions Department either via email: permissions@wiley.com or use the RightsLink service by clicking on the Request Permission link accompanying this article on Wiley Online Library (www.onlinelibrary.wiley.com).
Fig. 2: Image courtesy of Peter Erfurt & Prof. Dr. Thomas Lenarz, MHH Hannover, Germany.
- O’Connell, B.P., Hunter, J.B., & Wanna, G.B., (2016). The importance of electrode location in cochlear implantation. Laryngoscope Investigative Otolaryngology, 1: 169–174.
- Holden, L.K, Finley, C.C., Firszt, J.B., Holden, T.A., Brenner, C, Potts, L.G., Gotter, B.D., Vanderhoof, S.S., Mispagel, K., Heydebrand, G., & Skinner, M.W. (2013). Factors affecting open-set word recognition in adults with cochlear implants. Ear Hear. 34(3):342–360.
- Wanna, G.B., Noble, J.H., Gifford, R.H., Dietrich, M.S., Sweeney, A.D., Zhang, D., Dawant, B.M., Rivas, A., & Labadie, R.F. (2015). Impact of intrascalar electrode location, electrode type, and angular insertion depth on residual hearing in cochlear implant patients: Preliminary results. Otol Neurotol. 36(8):1343–1348.
- Wanna, G.B., Noble, J.H., Carlson, M.L., Gifford, R.H., Dietrich, M.S., Haynes, D.S., Dawant, B.M., & Labadie, R.F. (2014). Impact of electrode design and surgical approach on scalar location and cochlear implant outcomes. Laryngoscope. 124(6):1–7.
- O’Connell, B.P., Cakir, A., Hunter, J.B., Francis, D.O., Noble, J.H., Labadie, R.F., Zuniga, G., Dawant, B.M., Rivas, A., & Wanna, G.B. (2016). Electrode location and angular insertion depth are predictors of audiologic outcomes in cochlear implantation. Otol Neurotol. 37(8):1016–1023.
- Nordfalk, K., Rasmussen, K., Hopp, E., Bunne, M., Silvola, J.T., & Jablonski, G.E., (2016). Insertion Depth in Cochlear Implantation and Outcome in Residual Hearing and Vestibular Function. Ear Hear. 37(2):e129–137.
- Iseli, C., Adunka, & O.F., Buchman, C.A. (2014) Scala tympani cochleostomy survey: a follow-up study. Laryngoscope. 124(8):1928–1931.
- Ishiyama, A., Doherty, J., Ishiyama, G., Quesnel, A.M., Lopez, I., & Linthicum, F.H. (2016). Post Hybrid Cochlear Implant Hearing Loss and Endolymphatic Hydrops. Otol Neurotol. 37(10):1516–1521.
- Boyer, E., Karkas, A., Attye, A., Lefournier, V., Escude, B., & Schmerber, S. (2015) Scalar localization by cone-beam computed tomography of cochlear implant carriers: A comparative study between straight and periomodiolar precurved electrode arrays. Otol Neurotol. 36(3):422–429.
MED-EL
Was this article helpful?
Thanks for your feedback.
Sign up for newsletter below for more.
Thanks for your feedback.
Please leave your message below.
CTA Form Success Message
Send us a message
Field is required
John Doe
Field is required
name@mail.com
Field is required
What do you think?
The content on this website is for general informational purposes only and should not be taken as medical advice. Please contact your doctor or hearing specialist to learn what type of hearing solution is suitable for your specific needs. Not all products, features, or indications shown are approved in all countries.
MED-EL