MED-EL
Published Oct 01, 2021
Auditory Wellness in Active Aging: An Opportunity to Change the Field of ENT

2021 marks the beginning of the United Nation’s Decade of Healthy Aging, an initiative to support adults across the world to live fulfilling, inclusive, and healthier lives. We know that hearing loss can be a major barrier to achieving healthy and fulfilling final decades of life for many. In this article, we will explore how the aging population and rising prevalence of age-related hearing loss, or presbycusis, are likely to present new opportunities for hearing care professionals across the world.
New Clinical Opportunities for Adult Hearing Care
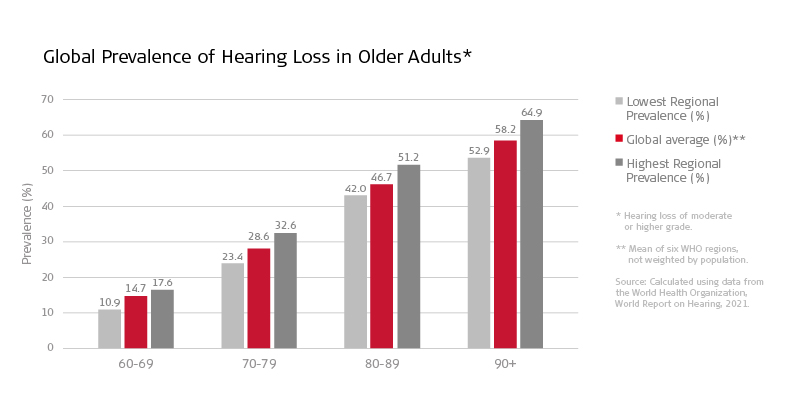
Now, with over 65% of adults over 60 living with some form of hearing loss[4], presbycusis could be the next big challenge for hearing healthcare professionals.
Senior Research Audiologist, Jane Opie, shares her thoughts on the opportunities this could bring for audiologists, speech and language therapists, and otologists:
“The release of the World Report on Hearing was an important moment as it crystallized how our professions can help to shape future hearing loss services. In many areas, access to hearing care professionals is critically low or severely underfunded. I believe that some of the key innovations of the future will be those that increase access to services for adults with untreated hearing loss, such as the following:
- Improving access to cost-effective adult hearing screening tools. This could be the first step to supporting adults to seek effective treatment.
- Creating novel approaches for alternative service delivery. Allied health professionals could bring basic audiology services directly to under-served communities.
- Reducing the reliance on centralized clinical-based interventions and effective referrals through digitally-led interactions that minimize travel time and costs.
- Researching core topics related to age-related hearing loss, particularly concerning cognition and other downstream outcomes, genetics, and maximizing patient outcomes.
- We expect that removing the burden on caretakers will also become an important topic in the future.”
The transition to translational and integrated healthcare has also helped to increase our understanding of hearing loss in adults and its connection to costly comorbidities. Research in this field has shown that untreated hearing loss in midlife is the number one modifiable risk factor for dementia, increasing the risk by 8%. This is followed by depression (4%) and isolation (4%), both of which frequently accompany hearing loss and are key barriers to active and healthy aging [2].
As auditory training is shown to have a positive impact on cognition [3], we also recently developed a free rehabilitation package for adults with CIs. The Adult Rehabilitation Kits (ARKs) support professionals to deliver auditory training, cognitive processing within listening practice, and the integration of hearing into a person’s lifestyle.
With a growing number of adults with hearing loss, tools like these and access to treatment will become increasingly important. We recognize that ENT professionals need access to the latest research, innovative best practices, and tools to meet these challenges.
To help clinicians assess the wider health factors of hearing loss, we’re developing a test battery designed to effectively screen and evaluate psycho-social-physical factors relevant to effective communication in older adults. We’ll share more news about this in a future blog. Make sure to subscribe to the MED-EL Professionals Blog so you don’t miss it.
Age Is Not a Barrier to Hearing Implantation
“Hearing devices are the treatment of choice for older people with hearing loss.”
World Health Organization [4]
But are implants the right choice for older adults? Significant improvements in hearing-related health outcomes have been shown in adults who receive hearing screening early followed by the use of appropriate hearing technologies [5-7]. Importantly, older age is not a contraindication for hearing implants, whether that be cochlear implants, BONEBRIDGE, or VIBRANT SOUNDBRIDGE systems.
Cochlear implantation in adults and older adults is proven to be safe, effective, and cost-effective [8-12], with people in their 90’s and beyond living with CIs. The use of local anesthesia for those deemed unsuitable for general anesthesia has been shown to not only shorten surgical time and the post-operative recovery period, but has helped increase access to hearing devices among older adults [9].
“I’ve always been a person who needs communication, both professionally and privately. With increasing hearing loss, however, every conversation became a horror. Constantly having to ask questions put me under enormous stress. At the age of 62, I got my first CI, and I got my second at 66. The operations went smoothly. I don’t want to go without my CIs anymore. I got my old life back, and now I can communicate magnificently again. The CI gave me more fun and joy in life once again.”
Gerhard, bilateral MED-EL cochlear implant recipient
Reported outcomes of hearing implants in older patients are also cited as being beneficial across both objective and subjective measures. Patients aged above 60 show post-operative audiological and speech discrimination outcomes similar to younger adults [13, 14]. Evidence also highlights significant increases in quality-of-life metrics of adults post cochlear implantation: Improved communication, social engagement, emotional, mental health, and physical well-being effects are among the wider outcomes recorded [15-18].
Auditory Wellness: A Journey Together
Over the coming years, we can each play a role in championing the importance of auditory wellness and active aging. We look forward to working with you to deliver focused research, innovative technologies, and digital solutions that support access to lifelong hearing care and auditory wellness for all ages.
References
- CGBD 2019 Hearing Loss Collaborators, Hearing loss prevalence and years lived with disability, 1990-2019: findings from the Global Burden of Disease Study 2019. Lancet, 2021. 397(10278): p. 996-1009. https://doi.org/10.1016/S0140-6736(21)00516-X
- Livingston, G., Huntley, J., Sommerlad, A., Ames, D., Ballard, C., & Banerjee, S. et al. (2020). Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet, 396(10248), 413-446. https://doi.org/10.1016/s0140-6736(20)30367-6
- Ferguson, M., & Henshaw, H. (2015). Auditory training can improve working memory, attention, and communication in adverse conditions for adults with hearing loss. Frontiers In Psychology, 6, 556. https://doi.org/10.3389/fpsyg.2015.00556
- World Health Organization, World Report on Hearing. 2021: Geneva. https://www.who.int/publications/i/item/world-report-on-hearing
- Mulrow, C. (1990). Quality-of-Life Changes and Hearing Impairment. Annals Of Internal Medicine, 113(3), 188-194. https://doi.org/10.7326/0003-4819-113-3-188
- Yueh, B., Souza, P., McDowell, J., Collins, M., Loovis, C., & Hedrick, S. et al. (2001). Randomized Trial of Amplification Strategies. Archives Of Otolaryngology–Head & Neck Surgery, 127(10), 1197-1204. https://doi.org/10.1001/archotol.127.10.1197
- World Health Organization. (2017). Integrated care for older people: guidelines on community-level interventions to manage declines in intrinsic capacity. World Health Organization. https://apps.who.int/iris/handle/10665/258981
- Spitzer, E., & Waltzman, S. (2021). Outcomes of cochlear implantation in adults over 85 years of age. Cochlear Implants International, 22(5), 296-302. https://doi.org/10.1080/14670100.2021.1913331
- Toner, F., Jackson, C., & Toner, J. (2013). How we do it: Local anaesthetic cochlear implantation. Cochlear Implants International, 14(4), 232-235. https://doi.org/10.1179/1754762812y.0000000016
- Gumbie, M., Olin, E., Parkinson, B., Bowman, R., & Cutler, H. (2021). The cost-effectiveness of Cochlear implants in Swedish adults. BMC Health Services Research, 21(1): p. 319. https://doi.org/10.1186/s12913-021-06271-0
- Laske, R., Dreyfuss, M., Stulman, A., Veraguth, D., Huber, A., & Röösli, C. (2019). Age Dependent Cost-Effectiveness of Cochlear Implantation in Adults. Is There an Age Related Cut-off?. Otology & Neurotology, 40(7), 892-899. https://doi.org/10.1097/mao.0000000000002275
- Chen, J., Amoodi, H., & Mittmann, N. (2014). Cost-utility analysis of bilateral cochlear implantation in adults: A health economic assessment from the perspective of a publicly funded program. The Laryngoscope, 124(6), 1452-1458. https://doi.org/10.1002/lary.24537
- Schafer, E., Miller, S., Manning, J., Zhang, Q., Lavi, A., & Bodish, E. et al. (2021). Meta-Analysis of Speech Recognition Outcomes in Younger and Older Adults With Cochlear Implants. American Journal Of Audiology, 30(3), 481-496. https://doi.org/10.1044/2021_aja-20-00141
- Speers, A., George, A., & Toner, J. (2015). An aging concern: A retrospective study comparing the audiological and speech outcome measures along with the surgical and quality-of-life outcomes in a group of geriatric patients with those of an adult control group. Cochlear Implants International, 16(sup1), S3-S5. https://doi.org/10.1179/1467010014z.000000000222
- Crowson, M., Semenov, Y., Tucci, D., & Niparko, J. (2017). Quality of Life and Cost-Effectiveness of Cochlear Implants: A Narrative Review. Audiology And Neurotology, 22(4-5), 236-258. https://doi.org/10.1159/000481767
- McRackan, T., Bauschard, M., Hatch, J., Franko-Tobin, E., Droghini, H., & Velozo, C. et al. (2018). Meta-analysis of Cochlear Implantation Outcomes Evaluated With General Health-related Patient-reported Outcome Measures. Otology & Neurotology, 39(1), 29-36. https://doi.org/10.1097/mao.0000000000001620
- Olze, H., Knopke, S., Gräbel, S., & Szczepek, A. (2016). Rapid Positive Influence of Cochlear Implantation on the Quality of Life in Adults 70 Years and Older. Audiology And Neurotology, 21(Suppl. 1), 43-47. https://doi.org/10.1159/000448354
- Sarant, J., Harris, D., Busby, P., Maruff, P., Schembri, A., Dowell, R., & Briggs, R. (2019). The Effect of Cochlear Implants on Cognitive Function in Older Adults: Initial Baseline and 18-Month Follow Up Results for a Prospective International Longitudinal Study. Frontiers In Neuroscience, 13. p. 789. https://doi.org/10.3389/fnins.2019.00789
MED-EL
Was this article helpful?
Thanks for your feedback.
Sign up for newsletter below for more.
Thanks for your feedback.
Please leave your message below.
CTA Form Success Message
Send us a message
Field is required
John Doe
Field is required
name@mail.com
Field is required
What do you think?
The content on this website is for general informational purposes only and should not be taken as medical advice. Please contact your doctor or hearing specialist to learn what type of hearing solution is suitable for your specific needs. Not all products, features, or indications shown are approved in all countries.
MED-EL