MED-EL
Published Jul 27, 2022
A Guide to Sound-Field Thresholds and Dynamics: Compression in MED-EL’s Cochlear Implant Systems

The sensitivity of a cochlear implant system governs the quietest sound level that results in usable stimulation for the implantee. This must be “just right” for a recipient to get the best benefit from their device.
Given the terms used in the title, we will begin with a couple of definitions:
- Dynamics relates to how the implant system translates the level of external sounds into electrical stimulation of a certain loudness.
- Dynamic Range describes the range between the lowest level and highest level that a system can process.
- Sound-Field Thresholds (SFTs; sometimes also referred to as free-field thresholds) relate to the quietest sound, presented via a loudspeaker, that can be reliably detected in a sound-treated environment. When talking about SFTs in the context of implant systems, we are normally referring to aided SFTs-detection levels when using the implant system.
Dynamic Range and Compression in Hearing Loss and Acoustic Hearing Aids
It is useful to be reminded of some of the issues faced by someone with sensorineural hearing loss (SNHL). SNHL is associated with a loss of sensitivity so that quiet sounds can no longer be detected. Therefore, a hearing aid applies gain such that quieter sounds can once again be detected. However, whilst sensitivity for quiet sounds is lost in SNHL, the loudness of higher-level input sounds is often relatively unaffected.
For example, a person with normal hearing might have a pure tone (audiogram) threshold of 0dB, and a maximum tolerable level of 100dB. A person with SNHL, might have a pure tone threshold of 70dB, but the same maximum tolerable level of 100dB, i.e., a dynamic range of 30dB vs. 100dB.
Thus, the individual may have limited dynamic range or recruitment, so if low-level and high-level sounds are amplified to the same degree, every day mid and high-level sounds may become uncomfortable. Hearing aids employ compression so that more gain is applied to lower-level sounds and less to high-level sounds.
Sound Compression in MED-EL Cochlear Implants
The situation for a cochlear implant user is quite similar: the dynamic range of electrical hearing is much narrower than that of normal hearing, and compression is required to allow the user to access the wide dynamic range of everyday sounds. In the MED-EL system, a multitude of parameters will influence the loudness perceived for a given external sound level. However, three are of primary importance for compression, with stronger effects than other parameters. (See Fig.1)
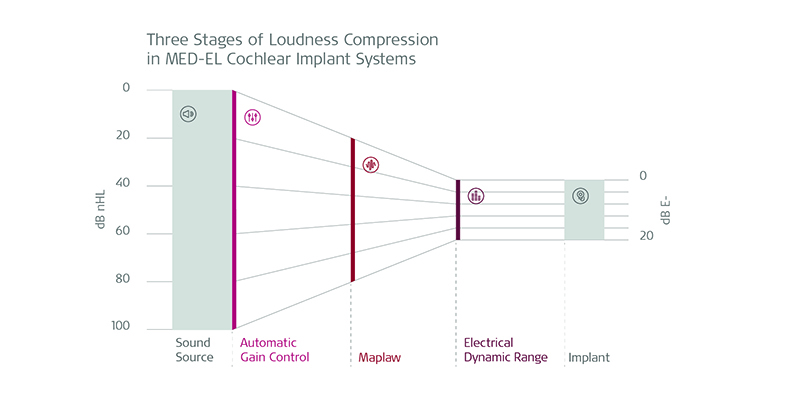
Fig. 1: The stages of compression in MED-EL cochlear implant systems
Three Key Parameters That Impact Loudness Perception
The first is the AGC (Automatic Gain Control). This acts quite like compression in an acoustic hearing aid: low-level sounds are boosted with high gain, whereas lower gain is applied at higher sound levels. One way of conceptualizing the action of the AGC is to picture it as a sound-level window that moves up and down the level range to best focus on the current overall level in the environment. Traditional AGC designs can compress speech signals well, but don’t handle sudden transients well (such as a slammed door or dropped crockery).
The MED-EL system uses a special “dual-loop” design to allow compression of speech but also responds well to transients. By default, the audio processor and MAESTRO fitting software employ relatively gentle compression characteristics, and a balanced sensitivity. These parameters provide a close emulation to compression processes in normal hearing, and additionally provide a relatively good match for compression characteristics for bimodal users (those using an acoustic hearing aid in the contralateral ear). However, the clinician can change these for particular cases if necessary.
The second parameter is an electrical loudness growth function, called “maplaw”. Essentially, this acts on the output of the AGC, compensating for the differences in response between electrical and natural hearing, to ensure a more natural change in loudness as the external sound increases in level. The default maplaw parameter produces good results for the vast majority of patients, but it can be altered if required in special cases.
The third parameter is the dynamic range which is defined between the THRs (highest undetectable stimulus levels), and the MCLs (Maximum Comfortable stimulus Levels). The maplaw function is ranged between these two points for each channel in the system. Of all the parameters considered for dynamics processing, accurate MCLs are the most critical in terms of the implant system delivering appropriate loudness cues, and therefore best performance. For most CI users, the THR parameter can be left at the default 8% of MCL, but in rarer cases, setting THRs accurately may be important.
MED-EL Cochlear Implants: Getting Dynamics Right
MED-EL’s engineers designed our cochlear implant systems with the avoidance of oversensitivity in mind to provide the best performance in everyday life. An individual should be able to hear quiet sounds without the system being oversensitive. Oversensitivity introduces low-level background sounds (such as fan noise from a computer, or distant traffic noise) that may become disturbing, or even interfere with ‘target’ sounds such as speech. Also, electronic systems (such as an audio processor) inevitably produce some internal electronic noise—called system noise. An oversensitive system could make this audible to the user.
The input dynamic range should be as wide as possible, to emulate normal hearing, and provide cues for level changes even at high input levels. This is important, as in noisy situations, we automatically raise our voice level to compensate for the environment. It is also important to avoid too much compression of mid-level sounds such as everyday speech, which could reduce or distort the dynamics cues available.
When these three criteria are combined, the MED-EL input-output function results in a target of ~30dB nHL as the lowest detectable level (or sound-field threshold), with ~100dB nHL as the upper limit of dynamic range. This also avoids the tempting, simplistic approach of designing a system to produce very low-level SFTs that appear to represent good performance but ignore the compromises that an oversensitive system will incur, such as poorer-than-ideal performance in noisy environments. Whilst quiet sound detection is important, it must be balanced against performance in everyday environments, such as classrooms or in a social setting with multiple talkers and noise sources.
Finally, this brings us back to the “just right” concept: In an under-sensitive system, quiet sound detection and performance will be poor, although there is some potential that noise is less disturbing in noisy environments. In an over-sensitive system, quiet sound detection may be very good, but noise will have a more detrimental effect whenever it is present. At MED-EL we aim for ‘just right’—the sensitivity of the system is balanced such that there is good quiet sound detection/performance, along with good performance in louder/noisier environments. Thus, the system delivers best performance for everyday life.
Sound-Field Thresholds Explained
One of the tests commonly used for fitting verification in hearing implant users is the determination of Sound-Field Thresholds, also known as the Free Field or ‘Aided’ Sound-Field test.
A proper Sound-Field test is one where the walls and furnishings have little or no effect on the sound and no reflections occur.
For sound-field thresholds both ASHA (American Speech Language-Hearing Association),[4] and the BSA (British Society of Audiology) have ‘guidance’ rather than a firm protocol.[5] What is common in these guidelines is acknowledgement of the limitations and the need to control an environment where there are unpredictable effects.
Ideally, all measurements would be made in a large (6 m x 4 m) soundproofed room with appropriate soft furnishing, with low ambient noise (measured according to ANSI S3.1),[6] a designated test spot and a fully calibrated loudspeaker set up (calibrated according to ISO 226:2003).[10] Pure tones must not be used due to the risk of standing waves (i.e. ‘hot spots’ of louder, and ‘cold spots’ of softer, noise). Warble tones or narrow band noise are appropriate and calibration guidance is available. If novel sound stimuli are used, consideration must be made regarding their calibration.
Because the quality and timing of auditory input differs for patients with cochlear implants, understanding the lowest level to which the recipient can respond is a fundamental step during the fitting process.
We also need to consider that when limiting the aided auditory evaluation only to tones (or narrow-band stimuli), there are two factors to consider:
- The audiometric frequencies commonly tested do not correspond to the frequency bands of the CI system, so ‘correcting’ the map based only on this information might lead to an incomplete solution.[9]
- Testing with speech stimuli, which are complex broadband signals, might generate a different answer than those given to for e.g., warble tones.
The Ling Test: A High-Quality Outcome Evaluation Tool
In addition, the Ling test should be administered as it can be considered a high-quality outcome evaluation tool that can be successfully implemented in a clinical setting.[1,3,8]
The test consists of six sounds spanning the speech frequency range. The ability to recognize these sounds is considered important as they incorporate energy across the speech frequency range from 250 to 8500 Hz, as typically occurs in running speech. It can be administered for detection or identification. The ability to detect these sounds can be used to determine if low, mid, or high-frequency sounds are audible in the aided condition. Identification includes this and also involves being able to name the presented sound and can help to assure good speech development, especially in paediatric patients.[2]
Audiometric Testing of Aided Hearing Threshold Levels in Cochlear Implant Recipients
Ideally, adaptive directionality in the audio processor should be switched off, but it would be a reasonable compromise to ensure the speaker in use is at 0 degrees azimuth (i.e. directly in front of the listener) and at least 1 m away from the listener. When this ideal environment is set up and calibrated, there is still uncertainty introduced by the presence of the subject themselves, parents, additional testers, toys, a table, etc.
In terms of test-retest reliability, Hawkins et al. showed that the between-session standard deviation (SD) of the aided SFTs measured on linear hearing aids was about 6-8 dB.[7] This means a test would have to differ by 12-16dB (two standard deviations) to be considered significantly different. This figure is widely accepted in clinical practice.
So, having outlined the limitations, MED-EL recommends:
Do Use SFTs:
- When frequency-specific (narrow band) understanding of the response may be useful.
- When the test subject is unable to do other tasks e.g. speech discrimination, speech in noise.
- When the subject is unable to report back fully.
- To identify the presence/absence of responses to sound.
- As part of a holistic assessment.
Do Not Use SFTs:
- As the sole test of implant outcome.
- To assume that speech/phoneme perception is adequate.
- As the sole verification of appropriateness of programming.
Best Practice:
- Ensure good response conditioning to the stimulus and avoid non-auditory cues.
- Use the best environment and equipment to which you have access.
- Consider the directionality of the microphones: have the recipient face the loudspeaker.
- Consider ‘front end’ processing; e.g. switch off front end features such as Adaptive Intelligence, etc. for the ‘purest’ result.
- Measure at the intended user volume and sensitivity.
- Note the test parameters for reporting and repeating (and expect this information in reports you receive).
- More compromises mean more variability.
- Use SFTs in combination with other tests such as the Ling Test to best assess aided performance.
Special thanks to Chris Durst and Fiona Kukiewicz from MED-EL UK as well as Alejandra Kontides and Jennifer Robinson from MED-EL Product Management for their contributions to this article.
Don’t Miss Any Updates From MED-EL
Make sure to subscribe to the MED-EL Professionals Blog to get MED-EL updates sent straight to your inbox as soon as they are published.
References
- Agung, K. B., Purdy, S. C., & Kitamura, C. (2005). The Ling sound test revisited. Australian and New Zealand Journal of Audiology, The, 27(1), 33-41.
- Goffman, L., Ertmer, D., & Erdle, C. (2002). Changes in Speech Production in a Child With a Cochlear Implant. Journal Of Speech, Language, And Hearing Research, 45(5), 891-901. https://doi.org/10.1044/1092-4388(2002/072)
- Glista, D., Scollie, S., Moodie, S., & Easwar, V. (2014). The Ling 6(HL) Test: Typical Pediatric Performance Data and Clinical Use Evaluation. Journal Of The American Academy Of Audiology, 25(10), 1008-1021. https://doi.org/10.3766/jaaa.25.10.9
- Sound Field Measurement Tutorial, Audiologic Evaluation Committee, Working Group on Sound Field Calibration
- British Society of Audiology. (2022). Practice Guidance – The Acoustics of Sound Field Audiometry in Clinical Audiological Applications. https://www.thebsa.org.uk/resources/practice-guidance-the-acoustics-of-sound-field-audiometry-in-clinical-audiological-applications/
- ANSI/ASA S3.1-1999 (R2018) – Maximum Permissible Ambient Noise Levels for Audiometric Test Rooms. (2018). https://webstore.ansi.org/Standards/ASA/ANSIASAS31999R2018?source=preview
- Hawkins, D., Montgomery, A., Prosek, R., & Walden, B. (1987). Examination of Two Issues concerning Functional Gain Measurements. Journal Of Speech And Hearing Disorders, 52(1), 56-63. https://doi.org/10.1044/jshd.5201.56
- Smiley, D., Martin, P., & Lance, D. (2004). Using the Ling 6-Sound Test Everyday. Retrieved 19 July 2022, from https://www.audiologyonline.com/articles/using-ling-6-sound-test-1087
- Quintana, A. K., Granados, M. P., & Cornejo, J. M. (2021). Calibrated Ling Sounds Test for Cochlear Implant fitting in children. In 2021 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), 1570-1572.
- ISO 226:2003 Acoustics — Normal equal-loudness-level contours. https://www.iso.org/obp/ui/#iso:std:iso:226:ed-2:v1:en
MED-EL
Was this article helpful?
Thanks for your feedback.
Sign up for newsletter below for more.
Thanks for your feedback.
Please leave your message below.
CTA Form Success Message
Send us a message
Field is required
John Doe
Field is required
name@mail.com
Field is required
What do you think?
MED-EL